Is there a link between mental health and gut health? Healthista spoke to The Gut Experts – Professor Barbara Ryan and Elaine McGowan RD. They reveal how managing your mental health can transform your gut health
Your brain is connected to every part of your body, so what is so special about the connection between your gut and your brain?
Well, it turns out that your gut enjoys a particularly intimate relationship with your brain, compared to the other important organs in your body, so much so, that the gut has been called your ‘second brain’ or the little brain.
While your brain contains about 100 billion neurones (nerve cells), your gut contains about 500 million neurones, which is impressive, given that your heart has only 40,000 neurones and your kidneys have about 1 million each.
an information superhighway that transfers information between the gut and the brain
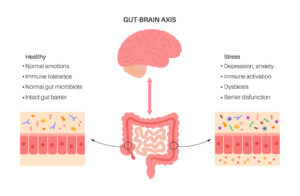
The gut-brain-axis (GBA) is the name given to this complex two-way flow of information and constant conversation taking place between your gut and your brain. It’s essentially an information superhighway that transfers information between the gut and the brain.
This means that what is happening in your brain (if you’re happy, sad, anxious or tired for example) can have a big effect on what is happening in your gut. And, equally, what is happening in your gut can also affect what is happening in your brain.
Three main communication channels make up your GBA: your nervous system which is the hard wiring between your gut and your brain; your immune system and your hormonal (endocrine) system.
Think of these as being the fast, medium and slower means of communication between the gut and the brain. The nervous system connects the brain to the enteric nerves (the nerves in the gut), via the vagus nerve and some other nerves that travel via the spinal cord.
Information transmitted via nerves travels very quickly and uses chemicals released from the nerve endings, called neurotransmitters. In return, information from emotional and cognitive areas in the brain (involved in the processing of thoughts, feelings and memories) is communicated to the gut.
The connection between mental health and gut health
Psychological stress, emotions such as anxiety, fear and anger and physical stimuli such as pain, can bring about changes in the functioning of the gut. These nerve signals can increase gut motility, which can result in diarrhoea, or they can slow emptying of the stomach, which can cause someone to feel nauseated or to vomit.
Those ‘butterflies in your stomach’ you may have experienced before a job interview or first date, or the need to dash to the bathroom when something nerve racking is about to happen – all those feelings are due to your GBA. The immune and hormone systems work more slowly than the nervous system, but also play an important role.
The nature of this incredible connection also means that looking after your mental health involves looking after your gut health, and looking after your mental health can have positive effects on your gut health. Researchers have since expanded the term to the ‘gut-brain-microbiota axis’, because of the important role your gut bacteria play in this process.
Beneficial gut microbiota (GM) produce a number of substances called short chain fatty acids (SCFAs), which have many important functions in the body, one of which is to act as a neurotransmitter in pain-pathways in the gut.
Science has proven the negative impact that stress and anxiety can have on a person’s digestive system
Other GM convert tryptophan, an amino acid present in foods to serotonin (95% of the serotonin in our body is produced by the GM), an important neurotransmitter that plays a vital role in the GBA and mental health. Having a healthy mix of GM can therefore directly influence our perception of pain in the gut and likely elsewhere in our body, and also our mental health.
A fascinating study called the SMILES trial showed that eating a Mediterranean-style diet for 12 weeks (a diet known to positively influence the GM) had a positive impact on mental health in people who suffered with chronic depression and anxiety.
Science has proven the negative impact that stress and anxiety can have on a person’s digestive system and wellbeing, and the impact is even greater in those with DGBI. Stress can also trigger flares in conditions such as Crohn’s disease or ulcerative colitis.
Because of the integral role of the GBA in gut health, it is not surprising that stress and anxiety can worsen any underlying gut condition. The good news is that taking even small steps to address these problems can have a positive impact on your digestive system and your general wellbeing.
A 2021 study published in Nature Genetics found that patients with IBS share a number of genetic pathways with people who have mental health conditions such as anxiety or depression.
This suggests that rather than IBS causing mental health problems or vice versa, that the long-recognised association between the two conditions might actually be due at least in part, to shared genetics.
READ MORE: IBS or SIBO symptoms? How to tell these common gut issues apart
How to tell if your mental health is causing your gut issues?
There is no one magic way to know if your symptoms are purely physical or if your mental health is playing a significant role in your gut symptoms, and there can be a combination of the two.
Because of the integral role of the GBA, gut symptoms can lead to mental health symptoms and vice versa. For this reason, it is important to discuss any new changes in your gut function with your doctor who will usually arrange some baseline tests to check for common ‘organic’ gut conditions.
There are some symptoms however that are strongly suggestive of the problem being predominantly a physical or ‘organic’ one, and these include:
- Nocturnal diarrhoea
- Recurrent mouth ulcers (these are associated with coeliac, Crohn’s and ulcerative colitis)
- Weight loss
- Swallowing difficulties
- Blood in the bowel motions
If you experience any of these symptoms, it is important to discuss this with your family doctor/GP.
What are the best ways to manage your mental health for gut health?
There is no special way of looking after your mental health specifically for your gut health. Different methods of nurturing mental health work for different people.
For some, regular exercise will improve mood, for others time spent in nature will help. For others more structured methods will help such as mindfulness, yoga, meditation, hypnotherapy or cognitive behavioural therapy (CBT).
Some top-line easy wins to look after your mental health to help nurture your gut health include:
- Diet: eating plenty of plant-based foods, rich in fibre will nourish beneficial GM and also have a potential beneficial effect on mental health.
- Exercise: regular exercise has been shown to be of benefit. 30 minutes 4-5 times per week can help.
- Alcohol: keep alcohol to a minimum: excess alcohol has a negative impact on the GM and is also associated with low mood.
- Sleep: it is vital to get sufficient, good quality, restorative sleep (7-8 hours is optimum).
Speak to your GP/ family doctor if you are experiencing significant mental health problems as in some cases where other simple steps are not working, medications may be required.
READ MORE: Why can’t I sleep? 8 reasons your gut health could be to blame
Our mental relationship with food – can stressing about what we are eating cause gut issues?
If you get unpleasant symptoms whenever you eat, then it is not surprising that you might start to dread eating and to worry about these symptoms coming on, even before you eat anything at all.
This is called ‘symptom anticipation’. The stress associated with anticipation of unpleasant symptoms can in turn affect the GBA, and the resulting increased anxiety can worsen gut symptoms. This has been described in both IBS and functional dyspepsia.
In an attempt to control their symptoms, people with gut conditions can often end up following increasingly restrictive diets and can develop quite rigid ‘food rules’. If they find themselves in a situation where they cannot control the content of their food (eating or visiting friends), the stress of breaking their ‘food rules’ can lead to worsening of their symptoms.
For this reason, some people with gut conditions end up avoiding social occasions or eating out, which in turn can have a negative impact on mood.
Professor Barbara Ryan and Elaine McGowan RD are The Gut Experts and authors of What Every Woman Needs to Know About Her Gut, published by Sheldon Press, £16.99
Follow The Gut Experts on Instagram @thegutexperts
Like this article? Sign up to our newsletter to get more articles like this delivered straight to your inbox.