It’s time to talk gynea stuff, and for the final installment of our new gynea series we discuss Polycystic Ovary Syndrome. Join us everyday for two weeks for expert advice on common intimate issues
Call them what you will – ‘women’s issues’, ‘intimate health problems’, ‘gynae things’, whatever, all women will experience at least one or two intimate conditions at some stage in their life.
Over the next two weeks, Healthista will be sharing some common intimate conditions many women experience but don’t talk about.
Here is what is helpful to know about some of the most common intimate issues, today we discuss Polycystic Ovary Syndrome (PCOS).
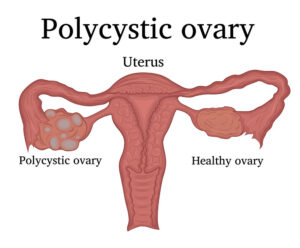
Polycystic Ovary Syndrome
PCOS is thought to affect one in 10 women in the UK although half of these are asymptomatic.
Women with PCOS typically have higher levels of ‘male’ hormones called androgens (like testosterone) which can affect ovulation, in fact you might not ovulate every month or at all.
This causes irregular periods, mood swings, weight gain, acne and hirsutism (thick, dark hair on their face, neck, chest, tummy, lower back, buttocks or thighs).
The ovaries often become enlarged and contain many fluid-filled sacs, or follicles, that surround the eggs and this condition can lead to problems conceiving.
Women with PCOS typically have higher levels of ‘male’ hormones called androgens
Women who have PCOS are often found to have higher than normal levels of the hormone insulin and are at greater risk of developing more serious health problems, particularly if they are overweight.
These include high blood pressure, type 2 diabetes, high cholesterol, heart disease and stroke and sleep apnoea (a condition where breathing temporarily stops when asleep).
Having PCOS can, understandably, lead to feeling down, depressed and impact on your self-esteem. Nobody knows exactly what causes it but having a family history of it and being overweight puts you at increased risk.
What can help:
There is no cure for PCOS but it can be managed. If you do have symptoms see your doctor who will discuss lifestyle measures including diet and exercise with you.
Other options include the combined oral contraceptive pill to help with erratic periods, facial hair and treat acne or may discuss rebalancing of the hormones and appropriate supplements.
Lifestyle-wise, if you are overweight losing some weight should help – exercise regularly, eat regularly to avoid blood sugar lows and eat a well-balanced diet which includes plenty of high fibre leafy green vegetables; lean protein like fish or skinless chicken and anti-inflammatory foods like oily fish, extra virgin olive oil and nuts and seeds.
Other options include the combined oral contraceptive pill to help with erratic periods
Avoid refined carbohydrates and processed foods like white bread, cakes, pastries, pies; sugary drinks and inflammatory foods which can affect how your body uses the insulin it produces.
Keeping your weight down will help reduce your risks of more serious illness like type 2 diabetes, heart disease and stroke and should also make you feel better about yourself.
More Healthista Content:
10 menopause symptoms myths debunked
Bad skin? Here’s what your spots are trying to tell you about your health
A gynaecologist’s guide to an irritated vulva
7 differences between migraine symptoms and a normal headache
Weak bladder? 9 tips to manage your symptoms
Like this article? Sign up to our newsletter to get more articles like this delivered straight to your inbox.