We have found the proven therapies, from those on the cutting edge of medicine to holistic solutions that work to fix headaches and migraines
Research from Headache UK found that chronic headaches strike a massive 10 million people in the UK, two thirds of them women aged between 20 and 50 making them the most prevalent and debilitating neurological condition in Britain. Alarmingly, the World Health Organization has classified migraine and severe headaches as among the top 20 causes of disability – up there with dementia, quadriplegia and active psychosis.
According to Professor Anne MacGregor, a leading neurologist and specialist in headaches in women at the National Migraine Centre, people tend to suffer in silence. ‘Up to 60 per cent of sufferers of chronic headaches never go and see a GP, despite the fact that now there is much than can be done to help their pain,’ says Professor MacGregor. One study conducted by the makers of 4Head (£4.95 from Boots), a topical headache treatment found that women put up with periodic attacks without seeking help for an average of 12 years!
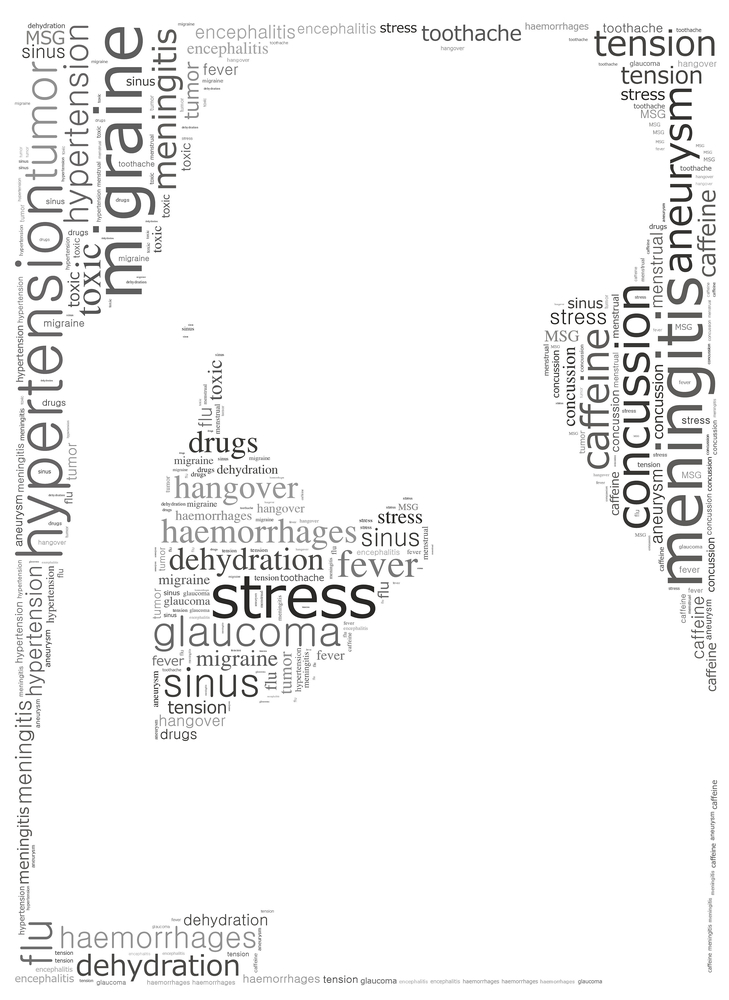
Is it a migraine or is it a headache?
According to Dr MacGregor, the same things that trigger headaches – most commonly stress, tension, tiredness, missing meals and dehydration – also trigger migraines. ‘The difference is that if you have a headache, a conventional treatment such as aspirin will alleviate the pain and allow you to continue with your day,’ she says. ‘If you have a migraine, such painkillers will not help, the pain interferes dramatically with functioning and you may need to go to bed.’
Most people don’t realise that their chronic headaches are more than likely migraines, says Dr MacGregor. ‘People get hung up on the idea of migraines always being on one side, but this is only the case in 60 per cent of sufferers,’ she says. Migraines will most often be accompanied by other symptoms including nausea, vomiting, sensitivity to light and noise and ‘aura’ before the headache starts which can manifest as zig-zag lines, slurred speech, dizziness and feelings of fear and confusion. ‘If your headaches make you feel sick or sensitive to light or they stop you from functioning, there is a good chance that you have migraine, so ask your doctor for a referral to a specialist headache clinic,’ advises Dr MacGregor. There are only 23 of these in the UK, five of which are in London so you may have to travel or pay privately for treatment. Ask your doctor if you are entitled to the treatment on the NHS.
Migraines run in families and new findings in the UK and Canada have identified a gene mutation associated with them that could one day lead to targeted drugs. But according to Dr Andrew Dowson, Director of Headache Services at King’s College Hospital, if your mother or father was a sufferer, you may be born with a genetic likelihood toward migraines but it’s not guaranteed you’ll develop them.
‘There has to be a certain number of factors that will work with that genetic susceptibility to trigger attacks,’ he explains. These include stress, infection or illness, sleep disturbances – too much or too little – hormone fluctuations, dehydration, skipping meals and flashing or flickering lights.
Could chronic headaches be something more sinister?
‘Daily headaches are the most common complaint in my practice,’ says West London GP Dr Carolyn Barshall. ‘People become anxious and worried that their persistent headaches are something more serious, such as an underlying brain tumour, but this is very, very rare and will usually occur with other dramatic symptoms such as sight or sense disturbances,’ she explains. The general rule she says, is to never ignore a headache that lasts more than ten days and, if the pain strikes suddenly and dramatically or is accompanied by other signs such as loss of sight or co-ordination seek help quickly.
According to Dr Dowson if you develop a sudden, excruciating headache having never suffered it before, seek help. ‘If it’s the first or the worst headache you have ever had and it has an accompanying rash or temperature it could be meningitis or a burst blood vessel in the brain, so get it looked at quickly,’ he explains. ‘But if someone has been getting headaches on and off for six weeks, six months or even six years it will be unlikely that they will have one of the serious underlying causes for headaches as these come with other symptoms that progress rapidly.’
In the vast majority, persistent headaches will be tension-type headaches, assures Dr Barshall. ‘These occur at the back of the skull and feel like a tight band around the head and neck and often develop as the day wears on, especially if people sit at computers in offices and get little fresh air.’ Stress, tiredness, poor posture, eye strain, alcohol – think hangover hell – as well hormonal changes can all cause such headaches. For more chronic headaches and migraines, here are the latest, effective ways to beat them.
NEW WAYS TO FIX YOUR HEADACHES
Botox for chronic migraines
Last year, Botox, a drug we know as the jab of smooth foreheads and ageless – often, expressionless – faces everywhere became the first licensed drug proven for the treatment of chronic migraine. Since then it has been revolutionising patients’ lives.
What happens ‘31 injections are placed at seven different areas in the head, the temples, forehead, top, crown, sides and back of the head as well as the top of the neck and shoulders,’ says Dr Brendan Davies, consultant neurologist at North Midlands Headache Clinic and trustee of the Migraine Trust.
‘We know it works but we don’t know exactly how. It probably suppresses release of pain-promoting chemicals in the brain that cause migraine. Once it has worn off after about 12 weeks, you will need to have another dose of the same amount.’
In case you’re wondering – we were – whether someone could have Botox for their wrinkles and get a ‘double-whammy’ effect of having their headaches disappear, they cannot.
‘The dosage in cosmetic use is very, very small, about 20 units and put into only in the forehead and face, whereas the amount administered for migraines is much higher, between 155 and 195 units, and put all around the head,’ explains Dr Davies. ‘There’s no evidence that Botox for wrinkles could make your headaches or migraines better.’
How to get it You will need a referral to a neurologist or specialist headache clinic from your GP and if they are convinced you need it, you will be entitled to receive treatment on the NHS. ‘To qualify for treatment, you will need to be getting at least 15 headache days a month, for at least three months and half of these need to be migraines,’ says Dr Davies. ‘As its an expensive treatment, your doctor will probably try other forms of preventative therapies first.’ These may include beta-blockers, tricyclic anti-depressants and drugs used to treat epilepsy that can prevent migraine attacks.
Supplements for migraine and headache
It’s rare for doctors to advocate holistic measures but when it comes to chronic headaches and migraines, many are convinced certain supplements can play a part. ‘Strong medications would be used for acute migraine attacks,’ says Dr Sam Chong, a consultant neurologist at King’s College Hospital. ‘But when it comes to long-term prevention, a holistic approach can be effective.’
What works There is good evidence Dr Chong explains, that Co-Ezyme Q10 reduces the frequency and severity of migraine. It works in the ‘mitochondria’ of cells where energy is produced so happily, many people report an improvement in their energy levels as well as their headaches. A study at Jefferson University found that migraine sufferers who took 150 mg daily could reduce the number of attacks they had each month.
‘Riboflavin, also known as vitamin B2, taken in the morning has also been shown to keep migraines and headaches at bay,’ explains Dr Chong. It’s not known exactly how it works but a three month Belgian study found that taking vitamin B2 cut headache attacks by over a third. Try taking about 400 mg of Riboflavin in the morning.
Other alternative treatments These include taking 400mg of magnesium a day as well as daily, low-dose aspirin and a herb called Butterbur, says Dr Dowson. ‘These are the five over-the-counter treatments proven to be helpful for headache patients,’ he says. ‘They won’t all work for everyone and people find taking some of these together may help them get control of their headaches. You might need a period of trial and error before you find something that works for you.’
The diet to help your headaches and migraines
You may have heard people with headaches and migraines being told to cut out red wine, chocolate, citrus fruits and cheese. ‘These contain natural chemicals called amines which include histamine, tyramine and phenylethyamine believed to trigger migraines,’ says leading nutritionist Dr Marilyn Glenville, author of The Natural Health Handbook for Women (Duncan Baird Publishing £16.99). ‘The theory is there should be an enzyme in our bodies that can destroy these substances but people who get migraines don’t have it.’
Although this theory became popular in the 1970s and 1980s, Sarah Haydon of the Migraine Trust, says there is no real evidence for dietary chemicals playing a part in headaches and migraines. ‘The most common dietary trigger we believe is not eating enough or skipping meals,’ she says. People who suffer with headaches and migraines need to eat regularly and keep their water intake high as hunger and dehydration are proven to trigger migraines in those with a susceptibility. ‘Moreover, there are certain symptoms that occur before migraines hit and one of these can be strong cravings for sweet foods and carbohydrates. This can lead people to eat chocolate or cheese and crackers before an attack and then blame the food for the migraine which was already on its way.’
What to do ‘Keep a diary,’ suggests Dr Glenville. ‘Write down what you have eaten in the 36 hours before a headache has struck. For many people it will take that long for a food to hit the liver and if the body is having trouble breaking it down, that’s when headache may strike. Also list stress, tiredness, where you are in your cycle as well as your water intake and the regularity of your meals. Do this for three months and you may become closer to identifying your headache triggers. Obviously if something sets off your pain, be it cheese or getting too exhausted, try and avoid it.’
6 TYPES OF HEADACHES AND HOW TO FIX THEM
Tension-type headaches
About a third of us get these regularly, usually felt as a tightening and pressure around the temples and back of the head, on both sides. They come on slowly and can last a few hours.
Solution ‘Check your water intake as these can be brought on my dehydration or by sitting in a stuffy office with few breaks,’ says Dr Barshall. If the pain persists, speak to your doctor who might suggest tricyclic antidepressants, not because you’re depressed but because they have been shown to lower the frequency, intensity and regularity of tension headaches. ‘As tension and poor posture are known to bring on such headaches, starting yoga can be helpful as it teaches you techniques to unclench the jaw and release tension in the shoulders and neck.’
Painkiller headaches
‘One per cent of women in the western world have medication over-use headaches,’ says Dr Chong. ‘People take painkillers to treat their headaches and then develop a dependency both physical and psychological. As they withdraw, another headache develops, they take more pills and the cycle continues.’ The most likely culprits are painkillers containing codeine which is highly habit forming and those with a combination of ingredients such as paracetemol or ibuprofen along with caffeine. ‘People think they have a headache when the painkillers wear off but it is their bodies wanting the substance such as caffeine topped up and responding with a headache,’ says Dr Chong. As little as two doses a week of painkillers containing caffeine can cause a dependency headache.
Solution ‘Don’t try and come off these by yourself,’ says Dr Chong. ‘Talk to your doctor and you can together work out a way of tapering off the painkillers to see if dependency is causing your headaches.’
Menstrual headaches
‘These can be related to the release of prostaglandin, the same hormone that causes heavy periods or, if the headache comes on in the two weeks before your period it may be related to dropping estrogen levels,’ says Dr MacGregor.
Solution ‘Doctors can prescribe estrogen patches to supplement dropping levels or may suggest a contraceptive that could switch off your natural cycle such as Depo-Provera, the progestogen only contraceptive injection or Mirena, a coil that releases hormones. Both can benefit women who suffer with chronic menstrual headaches,’ says Dr MacGregor.
Sinus headache
‘The most common misdiagnosis for migraine is sinus headache so this is less common than you might think,’ says Dr Davies. ‘As a result people may have costly operations and treatment on their sinuses when what they really need is treatment for their migraine.’
Solution If you have had a sinus infection you may experience a headache for up to a month afterwards, says Dr Barshall. ‘Help clear congestion by using a daily saline nasal rinse,’ she suggests. Try Sterimar, available from chemists (it’s brilliant for helping prevent colds too as viruses can breed inside your nose). Dr Glenville suggests looking at your diet. ‘Try removing remove both wheat and dairy from the diet as these two are the biggest congestion causing culprits and seeing if, after three months the facial pressure is better.’
Cluster headache
Four times more common in men, these affect one in 1000 people and are usually excruciating, brief, one-sided and develop suddenly. During each attack sufferers may also get redness and watering eyes, runny nose, sweating of the face, swelling or drooping of the eyelids and constriction of the pupils.
Solution ‘Where people with migraines want to be still, those with cluster headaches will usually want to pace,’ says Dr Mark Weatherall, consultant neurologist at the London Headache Centre. ‘Cluster headache is said to be the worst kind of pain.’ The key he says is to see your doctor to get a referral to a neurologist for a correct diagnosis. ‘During the bouts, migraine medication can work for cluster headaches but to be effective it will need to be taken as an injection or nasal spray. You may also be prescribed inhaled oxygen to have at home for fast relief.’
Sex headache
They’re not always an unimaginative way of getting out of sex. ‘If you get a headache in the lead-up to orgasm, it’s probably a tension type headache and nothing to worry about,’ says Dr Dowson. But if you get an intense headache during orgasm, it needs to be checked out by your doctor as that can be a sign of a sub-arachnoid haemorrhage or bleeding within the brain, he says.
Solution If you experience a headache during sex, discuss it with your doctor. If they are tension type headaches but severe, you may be prescribed medication. ‘If it’s was sudden and during orgasm – especially if your blood pressure is high also – see your doctor immediately who will refer you for a CT scan or other necessary investigations,’ says Dr Barshall.
For information and support contact The Migraine Trust on 0207 436 1336 or Migraine Action on 0116 275 8317
Like this article? Sign up to our newsletter to get more articles like this delivered straight to your inbox.